The Challenge
In Georgia, 80% of hospitals face high rates of patient readmissions and can be penalized with lower Medicare reimbursements as a result. Georgia patients struggle to receive appropriate levels of care, while hospitals and provider groups struggle to reduce readmission rates and receive adequate funding.
As a primary care group with a specialty division serving patients across South Carolina and Georgia, Your Health Inc. (Your Health, formerly known as SC House Calls) needed more granular data at the regional and departmental levels to effectively manage their care teams and track hospital admissions and readmissions to improve patient outcomes. With varied attribution between patients and providers due to the wide-ranging groups that may help just one individual, it was critical to better manage care teams of dietitians, therapists, transitional care managers and more. Additionally, the team wanted to effectively integrate key data to overcome logistical difficulties and administrative burden. Your Health was looking for a partner that could offer actionable data to facilitate incentives for transitional care management (TCM) visits and provide insight into metrics that would support decision-making in their value-based care programs.
The Solution
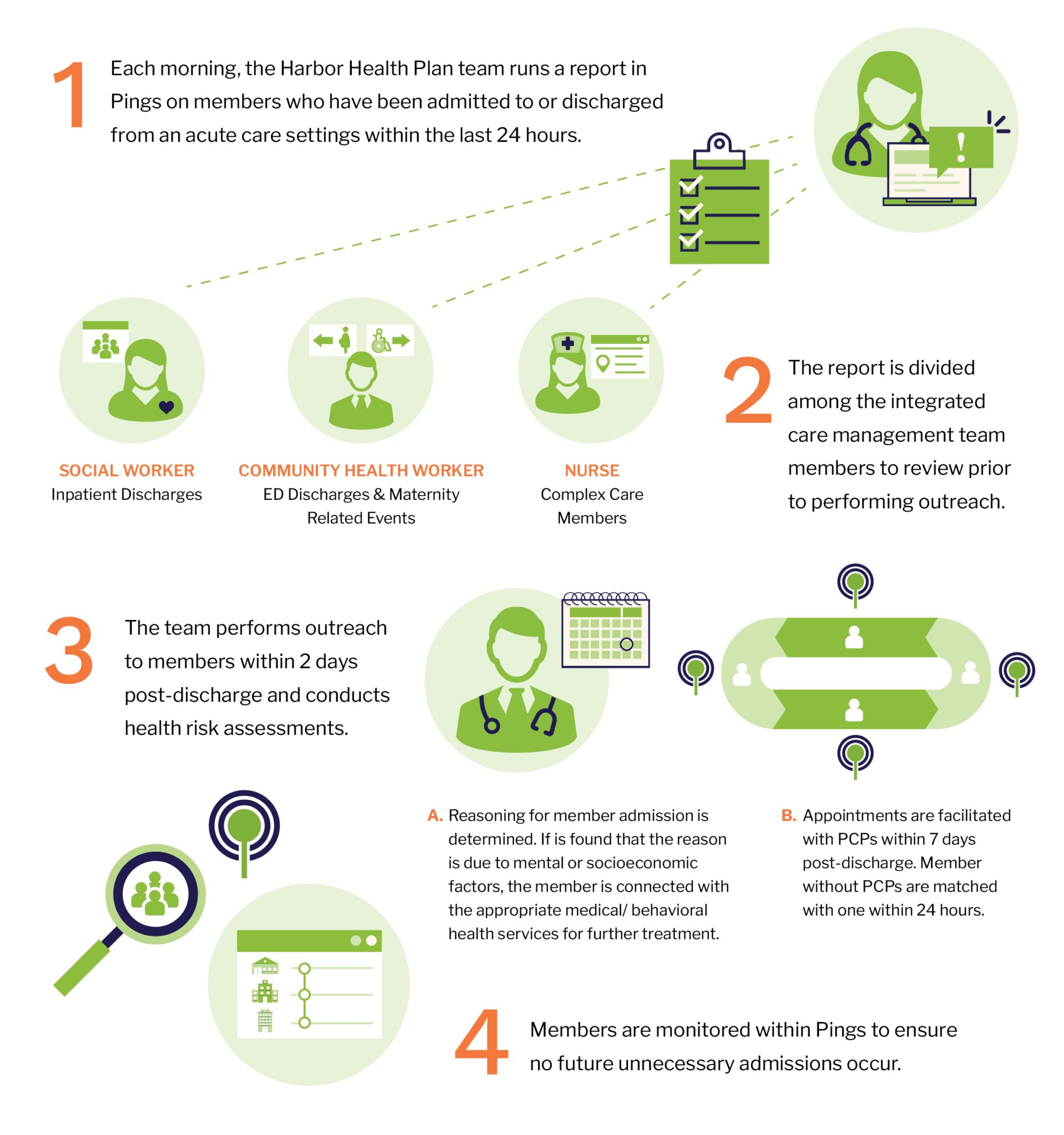
Your Health partnered with Bamboo Health to streamline data integration, improve care transitions and foster greater accountability across teams. The organization uses Bamboo Health’s Pings solution to support workflows that enhance patient outcomes, optimize resource allocation and align with value-based care initiatives.

“Bamboo Health allowed us to find details that traditional reporting would miss. Not just find those data points, but to actually be able to act on follow-up with patients and know where other care events happening with views into specific regions and specific care settings.”
David Clements Executive Director of Value-Based Care at Your Health
The Impact
By integrating with Microsoft Power BI, Your Health
was able to:
- Increase Accountability: Metrics for follow-ups within 48 hours and between 7-14 days were maintained above 90% compliance with payer requirements, a critical threshold for value-based contracts.
- Improve Real-Time Data Integration: With greater visibility into patient data and metrics, Your Health was able to visualize key metrics, track trends, identify areas for improvement and make data-driven decisions.
- Enhance Hospice and Home Health Management: Your Health used data insights to refine referral and follow-up workflows, ensuring patients received appropriate levels of care and reducing average length of stay.
- Empower Transitional Care Professionals (TCPs): With real-time data, Transitional Care Professionals (TCPs) can monitor and support patients throughout their hospital stay and transition to post-acute care by filtering alerts and notifications specific to the facilities they serve, enabling TCPs to serve as patient advocates even at partner facilities. This is especially important for Your Health, where TCPs are embedded in both SNFs and hospitals.

Bamboo Health allows us to have visibility into various care settings because we’re not always the one who sends or signs the order for patient care given that often the hospital sends it or the specialist sends it. Before Bamboo, we didn’t know when organizations were sending orders until the home health agency came 60 days after requesting an order to be signed, and we realized we could’ve been helping a patient 60 days earlier.
David Clements Executive Director of Value-Based Care at Your Health
The Results
Through improved data transparency and
streamlined workflows, Your Health has been able to:
- Improve follow-up measures by proactively managing care transitions and ensuring over 90% of patients receive follow-up care within 7-14 days
- Develop a more efficient, data-driven approach to hospice and home health evaluations, which has increased Your Health’s monthly home health evaluations from approximately 300 to over 1,200 per month
- Enhance TCPs’ impact as patient advocates, bridging communication gaps between patients and healthcare providers and allowing for more strategic planning and cost savings, including:
increase in home health revenue
decrease in hospice spend
decrease in home health spend
decrease in SNF spend
decrease in ED spend
reduction in cost to manage inpatient patients per month