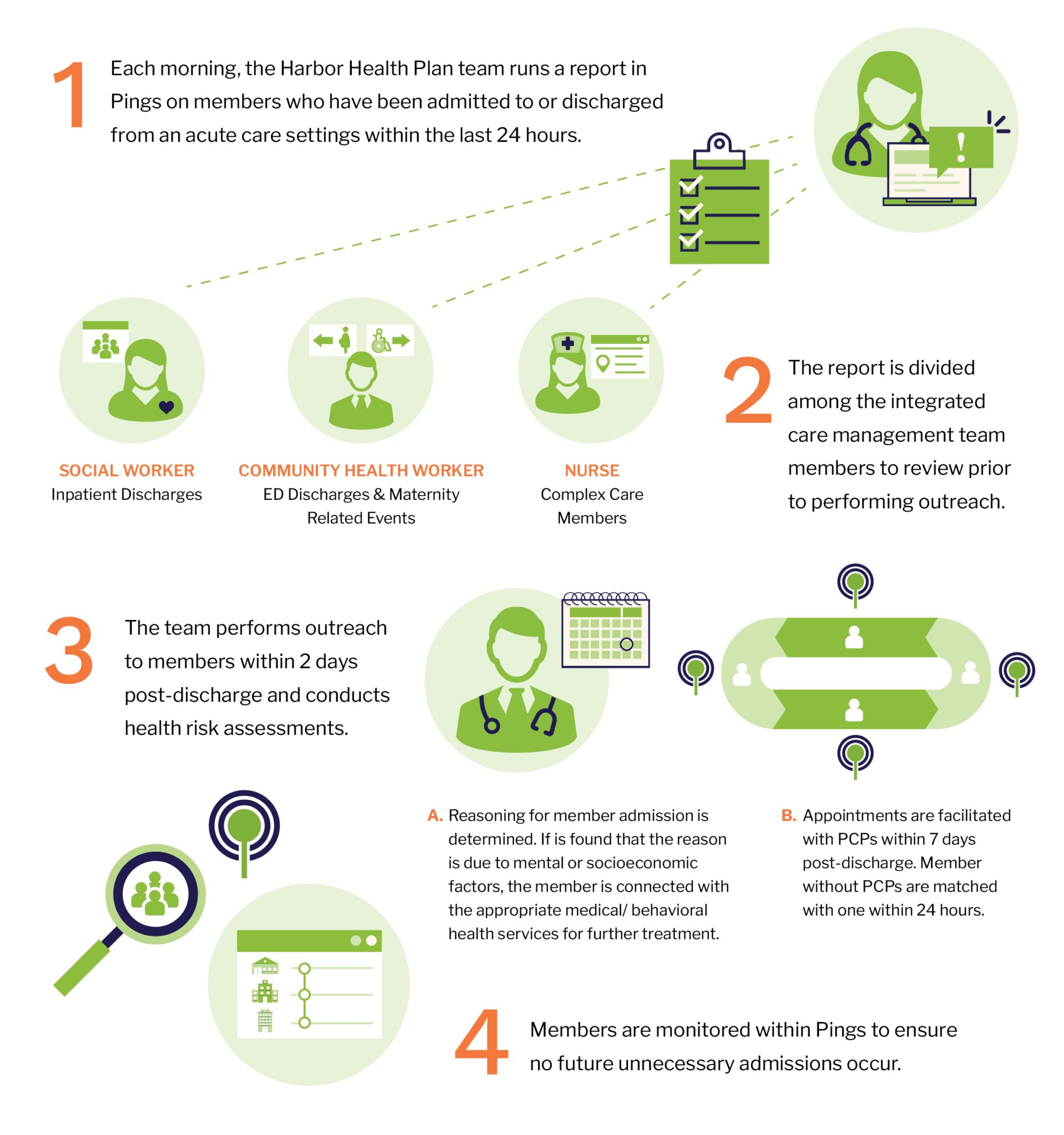
Each morning, Harbor Health Plan’s social worker runs a report in the Pings platform on members who have been admitted to or discharged from an acute care setting within the last 24 hours. The list is disseminated across team members, where the events are then color-coded and assigned to the appropriate person for follow up. Harbor Health Plan’s social worker is responsible for all inpatient discharges. The community health worker follows up on all ED discharges and maternity-related events, and the R. N. handles the events relating to complex care members.
The team has two business days to follow up with the member post-discharge to determine the reason for their admission, as well as to complete a health risk assessment. They then facilitate followup appointments with the member’s primary care physician (PCP). For members without an assigned PCP, the team will help to connect them with one within 24 hours, and schedule an appointment for them within seven days.
Daily reports allow care teams to monitor members who frequently present at acute care settings or may be at risk for readmission.
In many instances, the team finds that the readmissions are related to mental or behavioral health issues, lack of education on alternate settings where care can be received, a lack of PCP, or socioeconomic factors such as experiencing homelessness. The team will educate members,
connect them with medical and behavioral health services, develop care plans, or eliminate any other barriers the member might have to receiving care, in an effort to avoid further readmissions. Harbor Health Plan also uses the search feature in Pings to monitor any recent acute care events and continue outreach as needed.
After receiving a real-time Ping, the team will often intervene quickly by driving to the hospital or facility where the member is present. The team also uses Pings to learn more about the member’s care team. By having the care team contact information through Pings, Harbor Health Plan can reach out to them to discuss alternate care plans, prior visit histories, and any additional medical information, ensuring that the member receives the appropriate care.
Contact information for other care teams is available directly in workflows with Pings, so Harbor Health Plan can reach out to discuss alternate case options, prior visit histories and any additional medical information.