


2023
Impact
Report



2024 Healthcare Outlook
Let’s explore the key trends of 2024 shaping this transformation.

In 2024, we expect to see organizations moving towards IA, which will fuse automated insights with real-world healthcare knowledge. According to a Morning Consult survey from August, this shift is in the right direction. The report found that 7 in 10 U.S. adults are concerned about the increase in the use of AI in the healthcare industry, which underscores the need to partner humans and machines.




- 1
Intelligence Assistance (IA) to precede Artificial Intelligence (AI)
- 2
Connecting patients to the right care at the right time, without driving up costs
- 3
Continual evolution and adoption of value-based care (VBC)
- 4
Prioritization of social determinants of health (SDOH)
- 5
Flexibility with telehealth and brick-and-mortar care


1
to precede Artificial
Intelligence (AI)
In 2024, we expect to see organizations moving towards IA, which will fuse automated insights with real-world healthcare knowledge. According to a Morning Consult survey from August, this shift is in the right direction. The report found that 7 in 10 U.S. adults are concerned about the increase in the use of AI in the healthcare industry, which underscores the need to partner humans and machines.
2
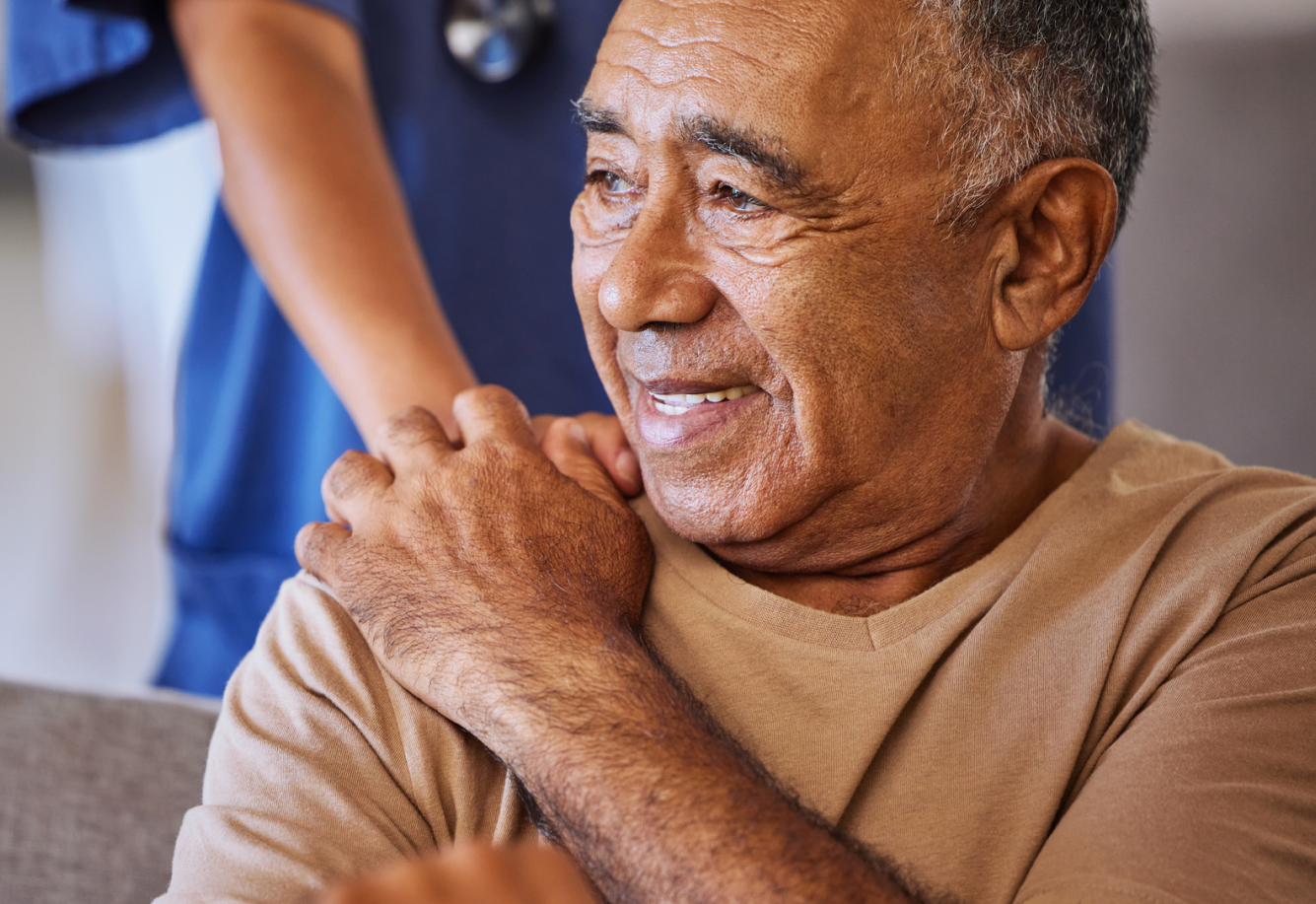
Overcrowding continues to burden the system as patients turn to the ED for substance use disorder and mental health challenges. As a result, outpatient care, such as behavioral health clinics, will continue to be a viable and necessary focus to reduce ED burden and connect patients to the longitudinal care they need most. Read more.




3
4
In 2024, we anticipate a greater focus on SDOH, especially in relation to rural communities. According to the Centers for Disease Control and Prevention, unintentional injury deaths, such as opioid overdoses and vehicle crashes, are approximately 50% higher in rural areas than in urban areas due to SDOH. These can include higher poverty levels, reduced healthcare access and environmental challenges. In the next year and beyond, state governments will need to prioritize how to address SDOH effects in rural regions by implementing policies that require healthcare providers to tangibly measure the impacts of SDOH and how to better integrate them in a person’s holistic care.




5
-
Acute & Ambulatory Providers
-
Pharmacies
-
Post-Acute
Facilities -
Hospitals
-
State
Governments -
Health Plans



47% Emergency Department Readmission Reduction
Pings improves ED burden for Massachusetts Community Health Centers’ 400,000+ patient lives.
Challenge:
- Increase visibility into ED visits for over 1 million patients with a diverse range of chronic issues
- Improve care coordination across 300 access sites
- Reduce instances where patients visit EDs not known to their providers


- 47%
reduction in 30-day
readmissions among
ED patients - 20%
drop in 30-day
readmissions - 33%
more follow-up care
30-days post-discharge
for hospitalized patients
Vicious Cycles to Virtuous Systems


Patient presents at ED:
32-year-old with suspected opioid overdose












Again, she receives immediate support for her overdose and care for her acute medical conditions, but doesn’t receive care for her underlying SUD and connection to ongoing SUD services (definitive assessment and treatment).

Again, she receives immediate support for her overdose and care for her acute medical conditions, but doesn’t receive care for her underlying SUD and connection to ongoing SUD services (definitive assessment and treatment).




Transitional Care
Management by 300%
and generate more revenue for the organization.
Bamboo Health’s Rising Risk won Best Care Management Solution Provider in the 2023 MedTech Breakthrough Awards.






Referrals in Nevada
- Improve access to behavioral health services through the state’s 988 Suicide and Crisis Support Lifeline
- Address the absence of a comprehensive referral system for individuals seeking mental health and substance use disorder treatment
- Optimize manual processes to promptly provide callers with a list of local resources for specific needs like food, transportation and housing


- 2172
referrals generated by CSSNV case managers in 2022
- 75%
of total OpenBeds®
referrals in Nevada
came from CSSNV - 39th
in the country for
overall access to
mental healthcare in
2022 (up 12 places
from 51st place in
2021) - 24+
other organizations in
Nevada utilizing
OpenBeds








Healthy Employees
breakdown
Bamboo’s Chief Clinical Officer, Nishi Rawat, MD, MBA, was named to Becker’s Healthcare’s Women in Health IT to Know list for the second consecutive year.